
Amniotic Band Syndrome
November 15, 2022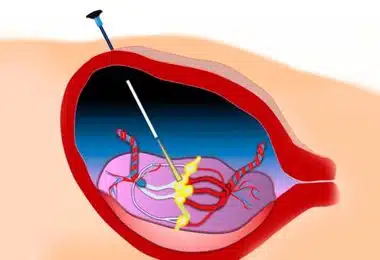
Twin-to-Twin Transfusion Syndrome
November 15, 2022
Amniotic Band Syndrome
November 15, 2022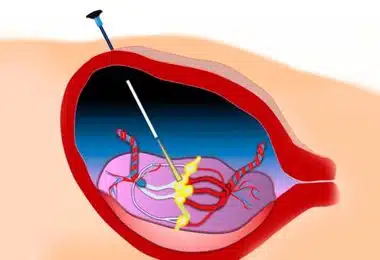
Twin-to-Twin Transfusion Syndrome
November 15, 2022
What Is Rh Incompatibility?
Contents
- What Is Rh Incompatibility?
- Are There Any Signs of Rh Incompatibility?
- What Problems Do Babies with Rh Incompatibility Have?
- How Is Rh Incompatibility Diagnosed?
- Is It Possible to Understand Whether the Fetus Has Developed Anemia?
- Can Anemia of the Fetus Be Cured By the Treatment of Rh Incompatibility?
- Are There Situations That Require a Blood Transfusion to the Fetus Other Than Rh Incompatibility?
Rh incompatibility occurs in pregnancies in which mothers are Rh-negative (Rh -) and fathers are Rh-positive (Rh+). Rh antigen can commonly be found in erythrocytes (red blood cells) of monkeys and much rarely in the ones of humans. The presence or absence of Rh antigens in humans should not be considered a disease. The problem occurs when an Rh-negative mother (Rh-) has a child with an Rh-positive partner (Rh+), and the baby’s blood type is Rh-positive (Rh+).
Are There Any Signs of Rh Incompatibility?
In couples with an Rh mismatch, the mother usually does not have any specific symptoms. However, in a situation where the fetus develops anemia and edema (dropsy) due to blood incompatibility, the mother may sometimes have a condition called mirror syndrome, when the mother may also have the same symptoms. Since in the case of Rh incompatibility, the fetus (the baby in the womb) suffers first, and mirror syndrome is pretty rare, waiting for the manifestation of this problem in the mother should not be a diagnostic method. The main symptoms of Rh incompatibility occur in the fetus and can only be diagnosed by ultrasound.


